CIRCULATORY SYSTEM DISEASE
CIRCULATORY SYSTEM DISEASE
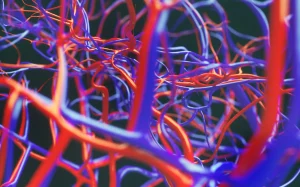
The circulatory system, also known as the cardiovascular system, is a complex network of blood vessels, the heart, and blood that circulates throughout the body. It plays a crucial role in delivering oxygen, nutrients, hormones, and immune cells to the organs and tissues, while removing waste products and carbon dioxide.
This intricate system ensures the proper functioning of all bodily systems and is essential for maintaining overall health and well-being.
Certain foods, herbs, and vitamins like carrot juice, ginger, vitamin C, and vitamin E may also support cardiovascular health. Incorporating a well-balanced diet that includes these beneficial components, along with regular exercise, maintaining a healthy weight, and avoiding smoking, can contribute to the maintenance of a healthy circulatory system.
Managing and addressing circulatory system disorders such as stroke, hypertension, coronary artery disease, heart attack, and peripheral artery disease is crucial to preserve the health and functionality of the cardiovascular system.
By taking proactive steps, one can support the well-being of their circulatory system and promote optimal overall health.
Description
The circulatory system disorder refers to various conditions that affect the cardiovascular system, including the heart, blood vessels, and blood.
Common disorders include hypertension, coronary artery disease, heart failure, arrhythmias, and peripheral artery disease. These conditions can lead to symptoms such as chest pain, shortness of breath, palpitations, and leg pain.
Diagnosis often involves medical evaluations, imaging tests, and blood tests. Treatment may include lifestyle modifications, medications, interventions (such as angioplasty or bypass surgery), and ongoing management to control risk factors and maintain cardiovascular health.
Circulatory system disorders can manifest through various symptoms, indicating potential issues with the heart, blood vessels, or blood circulation. Here's a closer look at some of the common symptoms associated with circulatory system disorders:
- Tachycardia: Tachycardia refers to an abnormally rapid heart rate, typically above 100 beats per minute at rest. It can be a sign of various cardiac conditions.
- Bradycardia: Bradycardia is characterised by an unusually slow heart rate, typically below 60 beats per minute at rest. It can result from issues with the heart's electrical system.
- Chest Pain: Chest pain, also known as angina or chest discomfort, can occur due to reduced blood flow to the heart muscle. It's often associated with coronary artery disease (CAD) or angina pectoris.
- Shortness of Breath: Difficulty breathing, or shortness of breath can result from reduced oxygen supply to the body due to circulatory problems or heart-related issues.
- Dizziness: Dizziness or light-headedness can occur when there is insufficient blood flow to the brain, potentially due to issues like low blood pressure or arrhythmias.
- Fainting: Fainting or syncope can be caused by a sudden drop in blood pressure or reduced blood flow to the brain, leading to loss of consciousness.
- Poor Circulation: Poor circulation can lead to symptoms such as cold extremities (hands and feet), swelling, and cramping, often associated with peripheral artery disease (PAD) or other vascular disorders.
- Numbness: Numbness or tingling sensations in the extremities may be a result of compromised blood flow, potentially due to conditions like atherosclerosis or blood vessel blockages.
- Nausea or Vomiting: Nausea and vomiting can occur as a response to pain or discomfort caused by circulatory system disorders, particularly in cases of heart-related issues.
- Confusion: Confusion or altered mental status can result from reduced oxygen supply to the brain due to poor blood circulation, as seen in conditions like stroke or transient ischemic attack (TIA).
There are many types of circulatory system disorders:
- Coronary Artery Disease (CAD): CAD is characterised by the narrowing or blockage of the coronary arteries, which supply blood and oxygen to the heart muscle. It can lead to chest pain (angina) or heart attacks (myocardial infarctions).
- Hypertension (High Blood Pressure): This condition occurs when the force of blood against the walls of the arteries is consistently too high. It can strain the heart and damage blood vessels.
- Heart Failure: Also known as congestive heart failure, this occurs when the heart is unable to pump blood effectively, leading to fluid build-up in the lungs and other parts of the body.
- Arrhythmias: These are abnormal heart rhythms. Conditions like atrial fibrillation (irregular heartbeat) and bradycardia (slow heartbeat) fall under this category.
- Peripheral Artery Disease (PAD): PAD results from the narrowing or blockage of arteries that supply blood to the limbs, typically the legs. It can cause pain, numbness, and reduced circulation.
- Deep Vein Thrombosis (DVT): DVT is the formation of blood clots in deep veins, often in the legs. If a clot breaks loose and travels to the lungs, it can lead to a life-threatening condition called pulmonary embolism.
- Aortic Aneurysms: An aneurysm is a bulge in the wall of the aorta, the body's main artery. If it ruptures, it can cause severe bleeding and is often fatal.
- Stroke: A stroke occurs when blood flow to the brain is disrupted, either due to a blockage (ischemic stroke) or bleeding (haemorrhagic stroke). It can result in neurological deficits and damage.
- Raynaud's Disease: This disorder causes narrowing of the blood vessels in response to cold or stress, leading to reduced blood flow to the fingers and toes.
- Cardiomyopathy: This refers to diseases of the heart muscle that can lead to heart failure or other complications.
- Vascular Malformations: These are abnormalities in blood vessels that can range from mild cosmetic concerns to serious medical conditions.
- Vascular Disease: A broader term encompassing conditions that affect blood vessels, including arteries, veins, and capillaries.
- Heart Valve Disorders: Conditions like valve stenosis (narrowing) or valve regurgitation (leakage) can affect blood flow through the heart.
- Endocarditis: Inflammation of the heart's inner lining, usually caused by bacterial infection.
- Thrombophlebitis: Inflammation of a vein along with the formation of blood clots, often occurring in the legs.
- High Cholesterol: Elevated levels of cholesterol can lead to the build-up of fatty deposits in blood vessels, increasing the risk of atherosclerosis and other circulatory issues.
- Ischemia: Ischemia refers to an inadequate blood supply to an organ or tissue, usually due to reduced blood flow. It can lead to tissue damage and is often associated with conditions like myocardial ischemia (reduced blood flow to the heart) or cerebral ischemia (reduced blood flow to the brain).
- Neutropenia: Neutropenia is a condition characterised by a low level of neutrophils, which are a type of white blood cell responsible for fighting infections. While it's related to the immune system, it can indirectly impact the circulatory system's ability to respond to infections.
- Angina: Angina is chest pain or discomfort that occurs when the heart muscle doesn't receive enough blood flow due to narrowed or blocked coronary arteries. It's often a symptom of coronary artery disease (CAD) and can be a sign of inadequate blood supply to the heart.
- Atherosclerosis: Atherosclerosis is the build-up of fatty deposits, cholesterol, and other substances on the inner walls of arteries. This condition narrows and stiffens the arteries, reducing blood flow and increasing the risk of heart attack, stroke, and other cardiovascular issues.
Circulatory system disorders can develop due to a combination of factors, and here are some common causes and contributing factors associated with these conditions:
- Ageing: The natural ageing process can lead to wear and tear on blood vessels, making them more susceptible to damage and narrowing, which can contribute to circulatory disorders.
- Genetics: Family history and genetic predisposition can play a significant role in the development of circulatory system disorders. Certain genetic factors may increase the risk of conditions like coronary artery disease, hypertension, or arrhythmias.
- Stress: Chronic stress can have adverse effects on the cardiovascular system, potentially leading to high blood pressure, heart disease, and other circulatory issues.
- Hormonal Changes: Hormonal fluctuations, such as those occurring during menopause in women, can impact blood vessel health and contribute to circulatory problems.
- High Cholesterol Levels: Elevated levels of LDL (low-density lipoprotein) cholesterol, often referred to as "bad" cholesterol, can lead to the accumulation of fatty deposits (plaques) in the arteries, increasing the risk of atherosclerosis and related disorders.
- High Blood Pressure: Hypertension (high blood pressure) can strain the heart and blood vessels, increasing the risk of heart disease, stroke, and other circulatory conditions.
- Lack of Exercise: A sedentary lifestyle can contribute to obesity, high blood pressure, and poor circulation. Regular physical activity is essential for maintaining cardiovascular health.
- Obesity: Excess body weight can lead to various cardiovascular risk factors, including hypertension, high cholesterol, and diabetes, all of which can contribute to circulatory disorders.
- Diabetes: Diabetes, particularly poorly controlled diabetes, can damage blood vessels and increase the risk of atherosclerosis, peripheral artery disease, and other circulatory complications.
- Smoking: Smoking is a significant risk factor for circulatory system disorders. It can damage blood vessels, promote plaque formation, and increase the risk of heart disease and stroke.
- Trauma: Physical trauma, such as injuries or accidents, can damage blood vessels or disrupt normal blood flow, leading to circulatory issues.
The medications listed are commonly used diuretics (water pills) that are often prescribed to manage circulatory system disorders associated with fluid retention and high blood pressure (hypertension). Here's a brief overview of these medications:
- Acetazolamide (Diamox): Acetazolamide is a diuretic primarily used to treat conditions like glaucoma and altitude sickness. It works by reducing fluid build-up in the body, including excess cerebrospinal fluid.
- Amiloride (Midamor): Amiloride is a diuretic that helps the kidneys remove excess salt and water from the body. It is often used in combination with other diuretics to help balance electrolyte levels.
- Bumetanide (Bumex): Bumetanide is a loop diuretic that is prescribed to remove excess fluid from the body in conditions like heart failure and oedema. It works by inhibiting the reabsorption of sodium and water in the loop of Henle in the kidneys.
- Chlorothiazide (Diuril): Chlorothiazide is a thiazide diuretic that helps the kidneys eliminate salt and water. It is used to manage conditions like hypertension, heart failure, and oedema.
- Chlorthalidone (Hygroton): Chlorthalidone is another thiazide diuretic that is prescribed for similar conditions as chlorothiazide. It can help lower blood pressure by reducing fluid volume.
- Furosemide (Lasix): Furosemide is a potent loop diuretic commonly used to treat conditions such as congestive heart failure, oedema, and hypertension. It helps the body eliminate excess fluid and salt.
- Hydrochlorothiazide (Esidrix, Hydrodiuril): Hydrochlorothiazide is a thiazide diuretic that works by increasing urine output, reducing fluid retention, and lowering blood pressure. It is often used to manage hypertension.
- Indapamide (Lozol): Indapamide is a thiazide-like diuretic prescribed for conditions like hypertension and oedema. It helps reduce excess fluid and salt in the body.
These lifestyle changes and natural approaches are indeed effective in promoting overall heart health and reducing the risk of circulatory system disorders. Here's a closer look at each of these recommendations:
- Regular Exercise: Physical activity is essential for maintaining cardiovascular health. Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity exercise per week, along with muscle-strengthening activities on two or more days a week.
- Well-Balanced Diet: Consume a heart-healthy diet that includes plenty of fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit saturated and trans fats, cholesterol, and sodium in your diet.
- Maintain Healthy Weight: Achieving and maintaining a healthy weight is crucial for reducing the risk of heart disease and other circulatory disorders. A balanced diet and regular exercise can help with weight management.
- Quit Smoking: Smoking is a major risk factor for heart disease. Quitting smoking can lead to immediate and long-term improvements in cardiovascular health.
- Limit Alcohol Consumption: Excessive alcohol intake can contribute to high blood pressure and other heart-related problems. If you consume alcohol, do so in moderation.
- Stay Hydrated: Proper hydration is essential for overall health. Drinking an adequate amount of water helps maintain blood volume and supports heart function.
- Good Sleep Habits: Aim for 7-9 hours of quality sleep per night. Poor sleep can contribute to hypertension and other cardiovascular issues.
- Hydrotherapy: Hydrotherapy, which involves the use of water for therapeutic purposes, can promote relaxation and improve circulation. Techniques like warm baths or contrast baths may be beneficial.
- Manage Blood Sugar Levels: For individuals with diabetes or those at risk of developing diabetes, managing blood sugar levels is crucial for heart health.
- Limit Caffeine Consumption: While moderate caffeine consumption is generally safe for most people, excessive caffeine intake can lead to increased heart rate and blood pressure in some individuals. Monitor your caffeine intake if you are sensitive to its effects.










