DIVERTICULITIS
DIVERTICULITIS
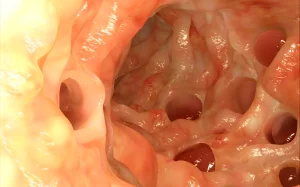
Diverticulitis is an inflammatory condition that affects the colon, specifically the small bulging bags or sacs called diverticula. It is characterised by inflammation and infection in the intestinal wall.
Symptoms include bloating, fever, abdominal pain, nausea, and changes in bowel habits. Risk factors include a low-fibre diet, sedentary lifestyle, and genetic predisposition.
Treatment involves antibiotics, pain management, and dietary adjustments. Resting the stomach, staying hydrated, and applying a heating pad can provide relief. Apples, broccoli, carrots, flaxseed, fish, and spinach, along with calcium, folic acid, and vitamin D, can support recovery. Diverticulitis primarily affects the colon, digestive tract, and abdomen.
Prompt medical attention is essential to prevent complications.
Description
Diverticulitis is an inflammatory condition affecting the diverticula, small pouches that form in the lining of the digestive system, usually in the colon. It occurs when these pouches become infected or inflamed, causing symptoms like abdominal pain, fever, nausea, and changes in bowel habits.
Diverticulitis can result from blockage of the diverticula by faecal matter, leading to bacterial overgrowth and inflammation. Risk factors include a low-fibre diet, ageing, obesity, and a sedentary lifestyle.
Treatment involves antibiotics, pain management, and dietary modifications, such as consuming a high-fibre diet and staying hydrated. Severe cases may require hospitalisation and, in some instances, surgery.
Early diagnosis and prompt medical attention are crucial to prevent complications like abscesses, perforation, or fistulas.
Symptoms of diverticulitis:
- Bloating or Gas: Many individuals with diverticulitis may experience abdominal bloating and increased gas production due to the inflammation and irritation of the intestinal lining.
- Fever: In cases of severe diverticulitis or when infection is present, fever may develop as a sign of the body's immune response to the infection.
- Shaking Chills: Fever accompanied by shaking chills can be a common symptom of diverticulitis, particularly when an infection is involved.
- Specific Pain in the Lower Left Abdomen: One of the hallmark symptoms of diverticulitis is localised abdominal pain, often concentrated in the lower left side of the abdomen. This pain can range from mild to severe and is usually persistent.
- Loss of Appetite: Many people with diverticulitis may experience a reduced appetite, which can be a result of abdominal discomfort, pain, and nausea.
- Nausea: Nausea is a common symptom of diverticulitis and can be accompanied by the urge to vomit.
- Vomiting: In some cases, diverticulitis may lead to vomiting, especially if there is significant inflammation or infection in the digestive tract.
- Tenderness in the Abdomen Region: The affected area of the abdomen, usually the lower left side, may be tender to the touch. Pressing on this area can elicit pain.
- Blood in the Stool and the Rectum: Diverticulitis can sometimes cause rectal bleeding, which may appear as bright red blood in the stool or on toilet paper. It is essential to seek medical attention if you notice blood in your stool, as it can have various causes, including diverticulitis.
- Constipation: While not always present, some individuals with diverticulitis may experience constipation, which can exacerbate abdominal discomfort and pain.
Diverticulitis can be classified into different types based on its severity and complications:
- Uncomplicated Diverticulitis: This is the mildest form of diverticulitis and involves inflammation of the diverticula without any significant complications. Symptoms may include abdominal pain, fever, and changes in bowel habits.
- Complicated Diverticulitis: Complicated diverticulitis refers to cases where the inflammation is associated with additional complications, such as abscess formation, perforation of the colon, or the development of fistulas (abnormal connections between organs).
- Perforated Diverticulitis: Perforation occurs when the inflammation leads to a small hole in the wall of the colon. This can cause infection to spread into the abdominal cavity, leading to a serious condition known as peritonitis.
- Abscess Formation: In some cases of diverticulitis, an abscess (a localised collection of pus) can form within or near the inflamed diverticula. This can cause pain, fever, and other symptoms.
- Phlegmon: A phlegmon is a localised area of inflammation and infection in the tissues surrounding the colon. It can lead to pain and discomfort.
- Fistula Formation: Fistulas are abnormal connections between different parts of the body. In diverticulitis, fistulas can develop between the colon and other organs, such as the bladder or small intestine.
- Pericolic Abscess: Pericolic abscess refers to an abscess that forms near the colon, typically in the tissues surrounding it.
- Recurrent Diverticulitis: Some individuals experience repeated episodes of diverticulitis. Recurrent diverticulitis may lead to chronic inflammation and scarring of the colon.
Causes and risk factors of diverticulitis:
- Genetic Predisposition: There is evidence to suggest that genetics can play a role in the development of diverticulitis. If you have a family history of diverticular disease, you may be at an increased risk.
- Obesity: Being overweight or obese is a significant risk factor for diverticulitis. Excess weight, particularly around the abdomen, can increase pressure on the colon and contribute to the formation of diverticula.
- Sedentary Lifestyle: A lack of regular physical activity and a sedentary lifestyle can contribute to constipation and slow bowel movements, increasing the risk of diverticulitis.
- Decreased Immune System Function: Individuals with weakened immune systems, such as those with certain medical conditions or taking immunosuppressive medications, may be more susceptible to diverticulitis and its complications.
- Medications such as Steroids: The use of medications like steroids can potentially weaken the intestinal wall and increase the risk of diverticulitis.
- Old Age (Over 60 Years Old): Diverticulitis is more commonly diagnosed in older adults, especially those over the age of 60. Age-related changes in the colon may contribute to its development.
- Smoking: Smoking is associated with an increased risk of diverticulitis. It can affect blood flow to the colon and contribute to inflammation.
- Excessive Consumption of Fats: A diet high in saturated fats and low in fibre may increase the risk of diverticulitis. A lack of fibre can lead to constipation and hard stools, which can contribute to the formation of diverticula.
- Low Fibre in Your Diet: A diet low in fibre is one of the most significant risk factors for diverticulitis. Fibre helps maintain regular bowel movements and prevents stool from becoming too hard, reducing the risk of diverticular formation and inflammation.
Medical treatment for diverticulitis:
- Antibiotics: Depending on the severity of the diverticulitis, your healthcare provider may prescribe oral or intravenous antibiotics to treat the infection and reduce inflammation. Commonly prescribed antibiotics for diverticulitis include:
Metronidazole (Flagyl): Effective against anaerobic bacteria often involved in diverticulitis.
Moxifloxacin: A broad-spectrum antibiotic that can target a range of bacteria.
Amoxicillin: Sometimes used in combination with other antibiotics to provide broad coverage.
- Pain Relief: Pain management is an important aspect of diverticulitis treatment, especially when experiencing abdominal pain. Over-the-counter pain relievers like acetaminophen (Tylenol) may be recommended to help alleviate discomfort. However, non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen are generally avoided due to their potential to worsen diverticular symptoms.
- Hospitalisation: Severe cases of diverticulitis may require hospitalisation, particularly if complications like abscess formation, perforation, or peritonitis occur. Hospitalisation allows for intravenous antibiotics, hydration, and close monitoring.
- NPO (Nothing by Mouth) and Bowel Rest: In some cases, healthcare providers may recommend a period of bowel rest, which involves fasting and refraining from eating solid foods for a specified time. This allows the inflamed bowel to heal and reduces stress on the digestive system. Intravenous fluids may be administered to maintain hydration.
- Surgery: Surgical intervention may be necessary for severe cases of diverticulitis or recurrent episodes that do not respond to conservative treatment. Surgery may involve removing the affected portion of the colon, a procedure known as a colectomy.
Natural treatment for diverticulitis:
- Liquid Diet and Rest: During a diverticulitis flare-up, it's often recommended to rest your digestive system by following a liquid diet. Clear liquids like broth, water, herbal teas, and clear juices can help reduce the workload on your intestines and provide essential hydration. Gradually introduce solid foods back into your diet as symptoms improve.
- Hydration: Staying well-hydrated is crucial during a diverticulitis episode. Drink plenty of water to prevent dehydration, which can exacerbate symptoms and hinder the healing process.
- Heat Application: Applying a heating pad or warm compress to your abdomen may help alleviate abdominal pain and discomfort. Heat can relax muscles and reduce tension in the affected area.
- Regular Physical Activity: Engaging in regular, low-impact physical activity can promote healthy digestion and overall well-being. Walking, gentle yoga, or other forms of exercise may help prevent constipation and support bowel regularity.
- Gradual Increase in Fibre: Once your diverticulitis symptoms have improved and you're ready to transition back to a solid diet, it's advisable to gradually increase your fibre intake. High-fibre foods like whole grains, fruits, vegetables, and legumes can help maintain regular bowel movements and prevent future diverticulitis episodes. However, make sure to consult with your healthcare provider or a registered dietitian to create a fibre plan tailored to your needs.
- Stress Management: Chronic stress can exacerbate digestive issues. Practices like meditation, deep breathing exercises, progressive muscle relaxation, and mindfulness can help manage stress levels and improve overall well-being.
- Avoid Trigger Foods: Identify and avoid specific trigger foods that may worsen your symptoms. Common trigger foods for some individuals with diverticulitis include nuts, seeds, popcorn, and high-fat or spicy foods. Keep a food diary to track which foods may exacerbate your symptoms.






